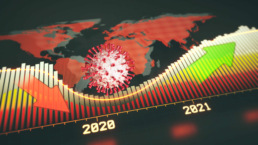
COVID-19 upended plans and left healthcare facilities scrambling to reorganize their day-to-day operations. Despite the unprecedented disruption, however, post-COVID trends in healthcare staffing look much the same as they did in 2019—only amplified.
Medely took a broad look at the marketplace as well as what healthcare workers and experts are saying to call out the top five healthcare staffing trends post-covid that facilities of all sizes should have on their radar:
- Healthcare leaders will implement COVID-sensitive strategies to improve retention
- Healthcare staffing will increasingly rely on data-driven recruitment
- Virtual health tools will have significant implications for staffing models
- Nurses and allied pros will expect action on diversity, equity, and inclusion
- Healthcare service providers will explore cooperative ecosystems
Here’s a look at each of these trends and what they could mean for your organization.
Staffing trend 1: Healthcare leaders will implement COVID-sensitive strategies to improve retention
Signing bonuses have become more over the past year, and salaries have gone up. But a year of juggling family time, work responsibilities, and personal wellness has shown many healthcare professionals that money isn’t always enough.
A Washington Post-Kaiser Family Foundation poll found that roughly 3 in 10 workers have considered leaving the healthcare profession. “More than half are burned out. And about 6 in 10 say stress from the pandemic has harmed their mental health,” reported William Wan.
To hold onto your best people, better support systems can make a significant difference.
Healthcare consultant India Owens, MSN, RN, CEN, NE-BC, FAEN, said practical interventions organizations could implement help to build frontline support systems. “Offering early and unlimited access to mental health care that is readily available and offered without reproach will be the key to survival for many nurses impacted by this tragedy,” she said.
Addressing professional concerns can also help nurses and allied professionals feel respected. Paying attention to career advancement opportunities, boosting staffing levels, and taking steps to alleviate safety concerns have all been shown to have an impact.
Finally, service providers will likely rely even more on recent graduates in the years to come. You’ll need to find a way to reduce the churn rate.
Pre-pandemic, nearly 33%of new nurses chose to leave the profession within the first two years, driven away by several factors: work environment, fear of injury, intense workload, emotional stress, and even a lack of support from their nursing colleagues.
All of these aspects have been compounded and made even more complicated by COVID-19.
Recognizing these difficulties is particularly important for nurses who are new to the workplace. “It will be important for healthcare organizations, professional development specialists, educators, and preceptors to be mindful of the disruption to their clinical education,” said one report that includes recommendations to help new nurses adapt.
Staffing trend 2: Healthcare staffing will increasingly rely on data-driven recruitment
According to the U.S. Bureau of Labor Statistics, the nursing profession is one of the fastest-growing professions in the country—and the number of new graduates hasn’t been able to keep pace. Significant shortages are projected for the next few years.
And that was before COVID-19.
Now the pandemic has driven the talent shortage to an even more concerning level. Per diem nursing and travel nurses have long been an effective way to close gaps, but the pandemic proved just how essential flexible expertise is. For more than a year, healthcare organizations have leaned hard on travelers to close critical gaps. The Washington Post reported that the number of open jobs for travel nursing peaked at 30,000 late last year—more than triple the norm.
Temporary staffing to that degree isn’t sustainable.
That means retention and job post fill rates are critical. And many organizations are getting creative to find insights they can use to get an edge and turning to technology for solutions.
From identifying regional imbalances—where some areas have a surplus of healthcare professionals and others have a deficit—to tracking down new graduates through LinkedIn and other social networks, learning how to find and analyze different types of data is essential if recruitment programs are going to succeed.
Staffing trend 3: Virtual health tools will have significant implications for staffing models
Telemedicine capabilities swelled during 2020. One study conducted by the CDC found that 95 percent of health centers reported using telehealth during the pandemic, compared with 43 percent in 2019. That’s a significant investment by providers to deliver patient-centered care in a safe, convenient, and often more effective way.
Critically for staffing considerations, it also requires fewer resources.
That’s a convenient option when demand for talent exceeds availability and budgets are tight as facilities wait for service delivery levels to return to normal. Virtual health offers a viable way to reduce overhead, reach more patients, skip unnecessary appointments and focus resources without compromising quality of care. And more technology is coming to improve patient care, from remote monitors to tech-driven scheduling.
Chad Mulvany, a director in the Healthcare Financial Management Association’s Washington, D.C. office, speculated about the potential impact:
“With fewer patients being seen in person, they’ll need fewer nurses and techs to triage them. And depending on the telehealth system used, the clinic may need fewer administrative support staff.
“While the system would probably want to keep a nurse and/or tech working virtually to act as care navigators/coordinators, they probably wouldn’t need as much clinical support staff and could redeploy them to other areas of the system.”
Chad Mulvany, Director in the Healthcare Financial Management Association’s Washington, D.C. office
For now, enhanced access to telehealth services is dependent on the temporary public health emergency (PHE) declaration for COVID-19. But many within the healthcare industry are pushing for a longer-term solution. In early May 2021, a bipartisan group of senators introduced legislation to set a foundation for telemedicine moving forward.
Staffing trend 4: Nurses and allied pros will expect action on diversity, equity, and inclusion
Improving diversity, equity, and inclusion in healthcare has been a priority for years. We know that better representation enhances the quality of care and ultimately leads to better patient outcomes.
And yet, 2020 has proven that there’s still a lot of work to be done. Within the U.S. healthcare system, COVID-19 has had a disproportionate impact on women and women of color in particular. It’s a group Karen Kahn, writing for Nonprofit Quarterly, called “the healthcare ‘underclass’”—nurses and allied pros whose occupations put them most at risk.
Finding a way to create better balance, particularly in the face of staffing shortages, is no easy feat. A report from McKinsey & Company said companies must focus on a few specific interventions that fit the current context and can have an impact. “There has never been as universal a need to reimagine working norms for all employees,” the authors wrote.
David Pedulla, an associate professor at Stanford University, said there’s no single answer—but there are solutions that have worked in the past. “Companies have the daunting task of figuring out what works … From counting, collecting, and comparing to accounting for complex organizational contexts, progress is possible.”
Staffing trend 5: Healthcare service providers will explore cooperative ecosystems
Igor Belokrinitsky, a partner with PwC’s Strategy, recently spoke on the “Next in Health” podcast about convergence he sees toward what he calls health ecosystems.
“One of the lessons of last year was that no one organization is big enough or strong enough to handle this crisis on its own,” Belokrinitsky explained. It’s become clear that efficacy requires collaboration with strong partners—an ecosystem within which you can share at multiple levels.
“[One] type of collaboration that we see is sharing of capacity,” Belokrinitsky said. For example, a facility could partner with other systems in a region to maintain one stockpile of protective equipment instead of several. Another example would be to share staff: “So in case of a natural disaster, for example, or some other urgent event, we can pull on people from other organizations in the region or in the state or even nationally,” he said.
Igor Belokrinitsky, Partner with PwC’s Strategy
There are barriers to such tight partnerships—including regulatory considerations. However, Boston Consulting Group said benefits such as improved access at scale, improvements in quality, lower costs, and the ability to allocate resources accordingly might appeal to those in the healthcare industry who see value in a more modular approach to doing business.
Conclusion
Many of the healthcare staffing trends post-covid exacerbated difficulties facilities were already dealing with. It’s also forced a lot of organizations to reconsider the status quo. By exploring new solutions and innovative ideas that have emerged over the past year, the healthcare industry will come out stronger on the other side. To get started planning for your post-COVID staffing requirements, sign-up with Medely today.